The story of Jana
For almost 39 years, I had no idea that I have this little cluster of blood vessels in my brain which looks like popcorn or a raspberry – until it decided to bleed causing a hemorrhagic stroke with left-side numbness.
Usually, Cavernoma are considered as not so dangerous because blood flow and pressure in these lesions are relatively low. However, the blood vessels do have thin and leaky walls and about 30% of people with Cavernoma have severe symptoms (like epilepsy and neurological deficits). Moreover, when it comes to a so-called overt hemorrhage it’s often a very life-changing event after which the majority of patients find themselves defining a “new normal”. Once a cavernoma has caused an overt hemorrhage, it’s more likely to bleed again – especially in the first 3-5 years after the first bleed. Currently, the only treatment is neurosurgery.
In my case, neurosurgery was not at all an option because it would cause more harm than good. So, I keep walking around with this little demon raspberry in my head hoping that it will behave now.
If it has taught me one thing, it’s the fact that I’m now more thankful than ever for every day to be alive.
Just about a year before my Cavernoma bled, I had started a coach/consultant business for electron microscopy and X-ray analysis in Germany. Then my husband got an offer for a position in Stockholm and we moved to Sweden. In our first winter here, in the morning of January 15th 2017, our kids (5 and almost 3 years old) were quite confused when, all of a sudden, I needed to be taken to the hospital because I couldn’t lift my left arm and couldn’t walk properly without support. At the hospital, the doctors couldn’t tell me whether I had a stroke or a tumor. I could feel that this situation was difficult for them as well and they tried everything they could to figure out what it was.
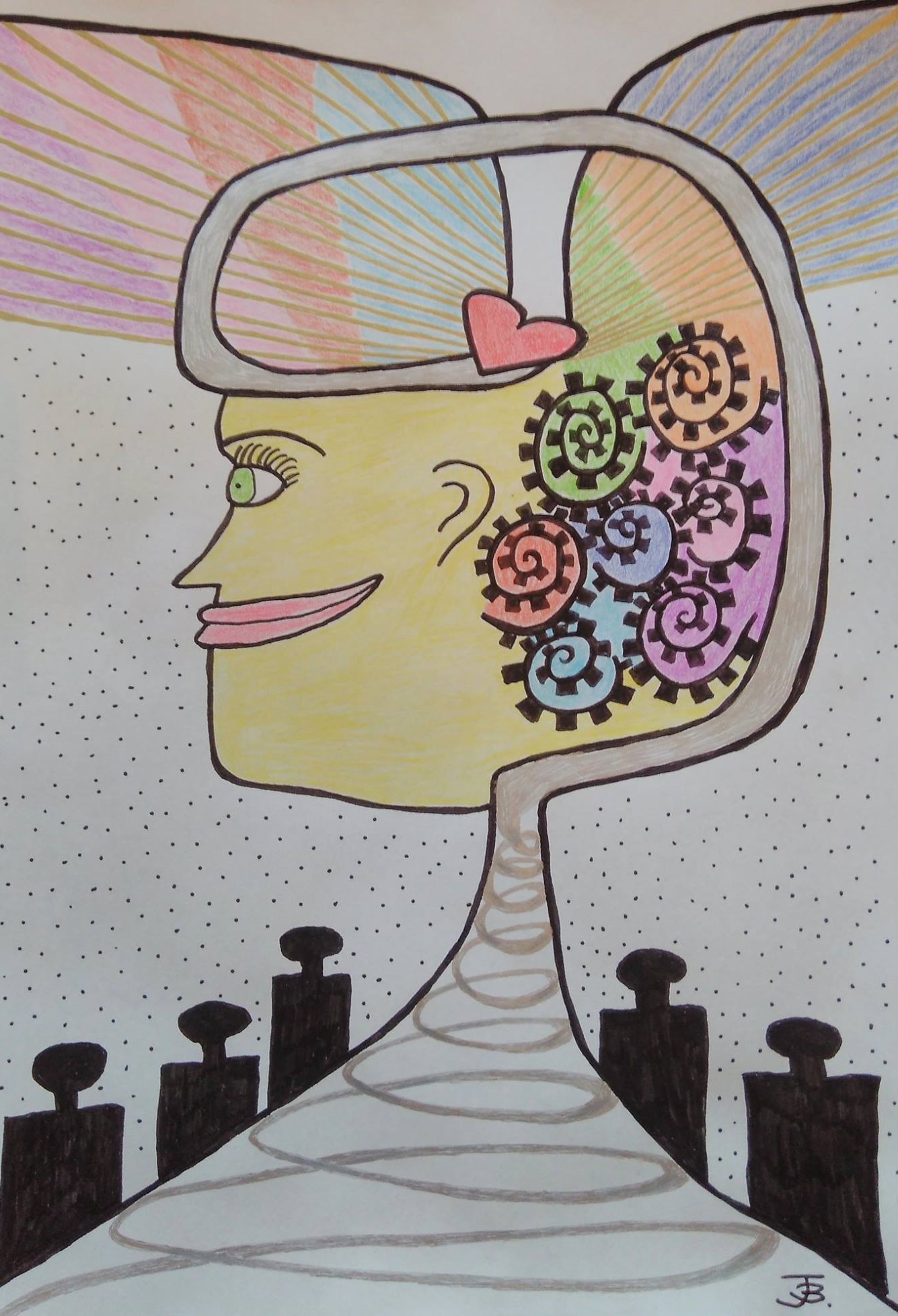
It took a CT scan, 2 MRIs, several blood tests, a lumbar puncture and in total 3 weeks until the hypothesis was raised that this might be a cavernoma. But again, surgery was not an option and otherwise there is no medication to keep cavernomas “under control”and stop them from bleeding. So, I ended up spending 8 months at home trying to recover and cope – painting helped me a lot to process the trauma, but also walking more and more every day.
The online community of Cavernoma patients was a place where I found comfort and support, because they understood well what I had gone through.
Now, after 3 years I’m not sure which trauma was bigger: the trauma of experiencing the symptoms and getting the diagnosis Cavernoma or the trauma of “falling between the chairs” in the health care system. Both together was probably a bit much at the time. In the beginning, it was not clear which department should take care of me – the stroke unit, neurology or neuro-oncology. The one phone number I got when I was sent home from the hospital belonged to a nurse who was very, very sorry to tell me that I apparently had the wrong number. The different doctors I got to see didn’t realize that the lumbar puncture results were actually never communicated to me – so, no wonder I was surprised when I found out (6 months later) about an atypical finding through ordering and reading my hospital records. These lumbar puncture results caused some uncertainty so that I had to be examined with MRI another 3 times in the first year.
In August/September 2017, when I was “cleared” of not having a tumor, I got some more help from the wonderful team at the Brain-Rehabilitation in Danderyd and then I slowly started working again. In the beginning I was working with upcycling and trashArt at Re:Innovation/Re:Unik in Täby, but then I became more and more involved in patient advocacy and was able to do a work training at Riksförbundet Sällsynta diagnoser/Rare Diseases Sweden. Together with other affected families, we started a Swedish patient organization (Cavernöst Angiom Sverige – CASE). In June 2019, eight national Cavernoma patient organisations came together for the first time to form the European Cavernoma Alliance with the goal to stimulate more collaborations between researchers, patients and clinicians in order to help find a cure for Cavernoma. As a more educated patient advocate, I also understand much better now, how stressful it must be to work in healthcare with limited resources and lots of administrative work.
So, now I can let go of all the frustration and replace it with energy that I can put towards improving the system.
And nowadays, I’m doing reasonably well. I can work part-time, I can manage my symptoms and I have found a new life purpose. At the same time, life itself is the mystery of all mysteries and who knows what happens tomorrow… The next MRI is just around the corner and I can’t wait to see how my lesion looks nowadays. I bet it will smile at me and say: “Keep going Jana, we will be fine!”
Cavernoma are also called Cavernous Angioma or Cerebral Cavernous Malformation (CCM). If more than one cavernoma is present, a thorough examination is needed, also of family members, because then the chances are high that it’s one of the rare familial forms (CCM1, CCM2, CCM3).